Latest News
Scared, angry, inept – that’s me, the carer
Icare. I’ve swapped roles with my wife and become a “carerâ€. When I had a stroke she was the “carerâ€. Now I have recovered, she has got cancer. It is my turn to do some “caringâ€. I suppose this must be the “until death us do part†stage of proceedings. I’m not sure I signed up for this bit – certainly not for this caring lark. I don’t want my role formalised in this way. It’s modern cant. Surely I’m only doing what a mate does. I don’t “careâ€. This has nothing to do with saintliness. I feel mostly rage, a savage impulse to howl at the moon.
Anyway, I’m lumbered. The hospital calls me a “carer†and I’ve got a little red card to prove it. “Chemotherapy Alert Cardâ€, it also says.
We learn that “the complications of chemotherapy are potentially life-threateningâ€. They include neutropenic sepsis. This can cause death, as it’s known in the trade.
I must contact the 24-hour helpline immediately if any of the following events occur.
“The patient has a temperature of above 37.5C.â€
I take her temperature continually. I’m rubbish at it. Jill gets irked. The process causes much tension. Then the temperature goes up. I get irked. I panic and ponder the helpline. The reading was “none†the other day. I had put the thermometer skewwhiff in the ear.
“Either you’re dead, or my watch has stopped.â€
This is no time for levity.
Or “if the patient feels shivery or flu-likeâ€. More than nebulous.
Or – get this – “if you feel generally unwellâ€. Come on. Pints of chemo and lashings of radiation and anyone might just feel a bit under the weather.
We’re never not going to be calling 999.
All this ambiguity is scary enough to prompt another stroke. My poor daughters will be charging around the hospital looking for their croaking parents in separate wards.
It started two months ago …
Jill, daughter Anna and I wander along to find out the results of the dreaded x-rays. “This is like death row,†mutters Jill. People come here every day to find out if they are going to die soon. What a life! We wait. And wait. Waiting in tropical, tense, insulting rooms is a huge part of caring. I blame that Hunt fellow. I glance at last year’s OK! or Hello! magazines. Jamie Vardy is presenting his baby.
Then we are softly summoned. An oncologist with a Giaconda smile calls us into a hushed room. A doe-eyed nurse stands by with a box of tissues. IÂ count silently to seven. My lucky number. Done it all my life.
Never works.
We make the smallest of talk, while mice click, computers twitch and x-rays surface on screens like creatures from the deep.
My goodness, there’s an elephant in the room.
Then the oncologist seems to say, “I’m afr …â€
Wham! That’s it. I hear the “F†and my mind seizes on it like a rat trap. “Afraid.†Then we seem to hear words like “confirmedâ€, “malignâ€, “mass in the lung†and “squamous cell carcinoma†– the ears don’t process them, the eyes blur, the mind goes dizzy. It feels fell, like Hopkins’s: “… cliffs of fall / Frightful, sheer, no-man-fathomedâ€.
The oncologist tenderly holds Jill’s hands. She weeps. Anna weeps.
The oncologist tells us this is by no means a death sentence. “There are ‘exciting’ developments in lung cancer.â€
I can do without this kind of excitement.
We say goodbye and then we all say nothing and wander back and curse things numinous and the random cruelty of the gods.
“But I never drank, smoked or drugged …â€
Jill is in the Kingdom of the Sick.
She will be “fighting†cancer.
Balderdash.
It is fighting her.
Jill’s treatment begins. For a month we catch the tube and thread the carcinogenic city streets to the hospital. She goes to “bloodsâ€. She gets weighed. She can’t lose weight. We must forget her diabetes and plump her up like a sumo wrestler. The chemo ward is full of bone-tired, gaunt and wasted patients being pumped with yards of poison by jolly nurses for hours on end. I bring Jill occasional coffeeless coffees and dying sandwiches. She doesn’t want them. Or me. So I visit a place where carers care for carers. It is cringingly well-meaning and full of women who nod a lot and say “yes†before I finish a sentence and suggest I go Nordic walking or attend a mindfulness course. That should do it. I return to find Jill in a deep stupor. I shake her alive in my now established caring manner.
“Come on! Time for your radiation.â€
She smiles at the horror of it all.
She must now be carted off to a dark, windowless dungeon for a blizzard of radiotherapy. She is given enough to poleaxe a rhinosaurus. Perfect storms of the stuff. I wait and wait and feel pointless. Jill returns after 15 minutes, dazed, fried and irradiated and we totter back home. Arm in arm, we negotiate the gridlocked streets. Our shrunk shanks can’t beat the green light on a pedestrian crossing and we are abused by a prime arsehole in a Range Rover.
“Cancer patient! Stroke victim. Carer! Fuck off!†we roar, maturely.
It makes us howl with laughter.
We resolve, whatever happens, to finally make that trip to New Orleans and dance under the light of a Cajun moon.
Jill lies most of the time in a foetal heap and I wake her up regularly for slugs of morphine. I ponder a nip. I then offer her doughnuts, Jammie Dodgers, fryups, bangers and mash or Jelly Babies. “Sod off!†I apply ice-cool flannels and offer mountain waters and she tells me the same. But she must drink fluids. She will die if she doesn’t.
We have water fights.
Still, we’re nearly there.
Only two weeks of this medieval farrago, this “caring†to go.
Then … Wallop! Catastrophe!
The two-year-old granddaughter discovers Jill upside down on a sofa. She thinks it’s hilarious. It’s delirious. Is it posthumous? Is this one of those complications of chemotherapy? Neutropenic sepsis? The carer steps in. 999! Ambulance round in seconds. Jill’s blood sugar levels are stratospheric. Something has gone mightily toxic. We zoom off to the acute ward. I’m told to scarper.
I visit next day at dawn. Jill is still hallucinating. She seems to be in a liminal state of waking and nightmare. I am very frightened.
Voices, almost disembodied, come at me in the crepuscular light.
“There were two figures at the end of the bed,†Jill confides.
Ah.
“They were priests.â€
Ah.
“They were saying, ‘At last you’re here, then.’â€
Christ.
Heaven. Hell. Charon and Cerberus?
Or her daughters, who have morphed into angels?
The figures were, of course, doctors.
One is talking to me.
“Are you the prime carer?â€
“Er … Yes.â€
“Are you next of kin?â€
Isn’t this a bit precipitate?
“Would you want her resuscitated?â€
Shut up!
It gets marginally better.
“We’ve done some brain scans.â€
Ah.
“And there are no traces of clotting or cancer.â€
I didn’t ask, but jolly good. Marvellous.
Blotto to all this, Jill munches on a mango stick.
It gets dreadfully worse.
A doctor returns.
He whispers at me: “Cancer traces in the brain.â€
This caring lark can be a bit of a rollercoaster – you don’t know if you are coming or going.
Twenty seconds later, the wicked messenger returns, antic, breathless, hysterical and apologetic, like Basil Fawlty.
“No! No! No! Forget it! There aren’t!â€
Whoops!
“I’m so so so so so so sorry.â€
“Typo!â€
As typos go, this is going it a bit.
I forgive him completely. I want to kiss the clot. Hug him. Relief trumps rage. Joy trumps despair.
Jill, still oblivious, continues to munch on another mango stick.
I pop out to find some water – or gin or crystal meth …
The blood sugar levels come down in two weeks and we’re let loose again into the world. Jill is now a fully fledged diabetic and I have fully fledged caring duties. Insulin. I’m now blood-sugar monitor. Tricky. I can’t get blood out. Maybe she has none left. At last, a trace! I take a reading. It’s ludicrously high. I summon a district nurse. She is great. I have been doing it wrong.
We Uber our way to the hospital for the final two weeks. Throughout it all, we have not risked the usual desperate questions about the dread tumour, disappearing, shrinking or spreading. How can an oncologist say or not say what we need to hear? Dispense fate with an x-ray? Break mortal news? How do patients hear it? In the kingdom of cancer, caution must rule.
So I walk on eggshells, more alert to a shiver of subtext, a lurch of semantics than in any excavations of some postmodern literary text.
“There is some evidence that the treatment is working.â€
We feast on this crumb. We ponder the semiotics of this scintilla of fact. We don’t dare take it further.
The NHS has been wonderful. Faults and weaknesses are a consequence of grotesque workloads and crippling fatigue. Random acts of senseless generosity are everywhere. They put my caring to shame. So do my daughters, who have been magnificent. The granddaughter is also a tonic. She still thinks it’s all a lark.
But I never realised it was such a slog. You’re multitasking 24/7 – morphine monitor, needle monitor, insulin monitor, blood-sugar monitor, temperature monitor, pill counter, chef, shrink, semantics analyst, blocker of prurient attentions, general shock absorber – among other things.
Still, “caring†is a breeze compared with the horror of being the patient.
All I care about it that we get out of this somehow alive, make that music trip to the Mississippi delta and dance to Cajun in New Orleans.

London’s most creative car park set to stay in heart of Peckham and remain open to the public
The council has been working closely with Bold Tendencies, the Peckhamplex Cinema and the team behind the soon-to-open Peckham Levels, to significantly extend their leases, which will ensure the former multi-storey car park remains a bustling, busy and sustainable part of the town centre and a London-wide cultural venue.
The site had been highlighted in the council’s New Southwark Plan, a blueprint for potential development in the borough, as an area to be re-developed for new mixed use development. However the most recent draft of the Plan, which is due to go to Cabinet for approval on Tuesday 31 October, has had the site removed.
Bold Tendencies said: “Southwark Council has worked a MIRACLE! We are lucky to have had the opportunity to develop our commissioning programme across visual art, architecture and classical music over the past ten years. This news only encourages us to do more work, to do it better and to reach more people in the borough and beyond!â€
Lodewijk van den Belt, Site Director at Peckham Levels, said: “Turning this multi storey carpark into a creative and cultural hub for Peckham and Southwark is proof that collaboration and creativity can deliver tangible results and opportunities in the local community. Peckham Levels is looking forward to working with Southwark Council, Bold Tendencies and Peckhamplex to create a unique destination and community asset and the extension of the lease guarantees a long term cultural legacy that will deliver genuine opportunities to all the creative entrepreneurs of Peckham.”
John Reiss, chairman at Peckhamplex, said: “Peckhamplex is delighted that the long time uncertainty over redevelopment of the multi-storey former car park has been postponed for at least 20 years. This will allow the directors to consider investment in the multiplex to enhance the offering to our loyal customers. We intend to keep providing a broad range of films at affordable prices. I look forward to continuing to work with Southwark Council on enhancing the cinema building and surrounding area to make it truly inviting for visitors, and developing the cinema’s offer to continue to attract customers from across the borough and the rest of London.â€
Cllr Mark Williams, cabinet member for regeneration and new homes at Southwark Council, said: “As an unused car park we thought this site had more potential through re-development. However following extensive consultation with local residents and recognising the fantastic work carried out by Bold Tendencies and Peckhamplex, and with the exciting new project at Peckham Levels, we have decided to secure the future of this site in its current form for the longer term. The council has been working closely with the three main cultural organisations using the car park to agree longer-term leases, paving the way for the building to remain a key part of the cultural activity that has put Peckham in the creative heart of the borough, and London.â€
Over the past 10 years, Bold Tendencies – together with its partner projects The Multi-Story Orchestra and Frank’s Cafe – has attracted over 1.5 million visitors to its annual summer project at its rooftop home. Its activities take place both onsite and offsite. Â Bold Tendencies animates its commissioning programme and the site for schools, families and the neighbourhood through standalone education and community programmes that take culture and civic values seriously. This summer 365 primary school age children participated in MY MUSEUM, an art and project space which trains young people to curate and take the lead in their own learning, and since 2014 120 young people have been part of the Bold Art Trainee Programme. Bold Tendencies will aim to continue to deliver excellence in its summertime commissioning programme, widen its attending audiences, in particular into Peckham and across Southwark, and remaster the site, working with some of the most significant emerging and established architects to design and commission new facilities and services on-site, bolting onto the existing fabric of the building and bringing into use of aspects of the site year round.
Peckham Levels is undergoing its final touches and is set to open the public on Friday 8 December 2017. It will comprise 50 studio spaces for artists, makers and small businesses, a number of co-working and workshop spaces, event venues and independent food, drink and retail business spaces. Ten of the studios will be let at subsidised rents to support emerging talent from the local area, and event and meeting spaces in the building will be available at low community rates at least 25% of the time, offering a new venue for community events, local meetings and charity fundraising.
All tenants will commit to give time weekly into a community investment scheme and 10% of net profits reinvested back into community projects. Â Already largely let, following a hugely successful member and operator application process, over 500 people will work in the building on opening day.
In addition, confirmation of the extended lifespan of the building will allow the owners of the Peckhamplex cinema, which also forms part of the building, to look at options for improving its facilities whilst continuing to deliver low-cost cinema tickets for local residents. The cinema attracts around 10,000 customers a week largely from the local catchment area but more recently from across London attracted by a broad and current offering of films at affordable prices.

Invisible and in distress: Prioritising the Mental Health of England’s Young Carers
The report highlights recommendations based on discussions with young carers, sector leaders and young carers services in the Carers Trust network.
Invisible and in distress: prioritising the mental health of England’s young carers (PDF, 1.3MB) found that while young carers frequently report that their caring role can cause distress and impact on their mental health, there are gaps in support and there are barriers that prevent them from accessing the support that they need.
Key findings
- Nearly half of the young carers in the survey (48%) said that being a young carer made them feel stressed and 44% said it made them feel tired.
- A different survey of 61 young carers in school found that 38% had mental health problems.
- The demands of their caring role and their family’s circumstances were often one of the reasons they found it difficult to access support, from the difficulty of arranging appointments without help from a parent, to worrying about revealing that they are “not good enough†to care for their family member.
- The criteria for accessing Children and Adolescent Mental Health Services can discourage young carers from getting support so that problems become even harder to tackle and cause more harm.
Key recommendations
- Caring roles amongst children and young people should be seen as a risk factor for their mental health.
- NHS England, the Department of Health, mental health trusts and local authorities can implement frameworks developed by Carers Trust, such as the Young Carers in Schools programme or Triangle of Care for Young Carers to ensure that the right information and support is given to young carers. They should ensure that they meet their duties to support young carers under the Children and Families Act 2014 and Care Act 2014.
Download the full report to find our more detail on the key recommendations (PDF, 1.3MB)

Carers UK responds to CQC’s report, State of Care 2017
 In response, Emily Holzhausen OBE, Director of Policy and Public Affairs at Carers UK, said:
“It is heartening to see that the quality of some care services is improving in response to inspection and regulation.
However, we are gravely concerned by the strain placed on the NHS and social care, which has resulted in reduced services, longer waiting times, fewer families receiving support, and an added pressure on beds affecting hospital discharge.
Carers UK sees first-hand the pressure this places on families, affecting work, health, and relationships.  We know that access to good quality care affords carers with peace of mind, especially when arranging the respite which is often integral to their own continued physical and mental wellbeing. Yet, our own research shows that one in four (25%) carers have not had a break in five years.
This is not sustainable for families, now or into the future. There is even greater urgency for Government to bring forward a settlement for social care for the short, medium and long-term.â€

Auto-enrolment means you must now set up a pension for your nanny or carer
Auto-enrolment went live on 1 October 2012 and requires all employers to automatically enrol eligible workers into a workplace pension where both the worker and their employer pay some money in. To date, more than 8.5 million people have been enrolled, many of whom will never have saved in a pension before. Workers can “opt outâ€, ie, say no to being put into the pension scheme. But they can’t do so until after they have been enrolled.
Big companies such as supermarkets were the first to sign up to the regime, but more recently the focus has switched to the millions of small and “micro†employers. As the Pensions Regulator puts it: “If you employ just one person, then you are an employer and have ‘duties’ under pensions law.â€
Of course, many of the smallest employers don’t think of themselves as such – they are individuals who just happen to have someone who works for them. That includes families who employ a nanny and people who employ a personal care assistant to help them with their day-to-day needs (if you pay for a personal care assistant using your own money, or money provided by your local authority or the NHS, you are judged to be an employer). Under the rules, many of these “employers†will have to set up a pension plan for their nanny/carer, and pay into it.
Employers must automatically enrol any employee who, on the date the law applies to them, is at least 22 years old but below state pension age; earns more than a minimum amount (currently £10,000 a year, the same as £833 a month or £192 a week); and is not in a workplace pension scheme. Some nannies and personal care assistants won’t meet these criteria because they don’t earn enough.
Up until now, employers have typically been given advance notice of the date when their auto-enrolment duties come into effect. This was known as their “staging date†and gave people time to get their ducks in a row. Previously, many employers received an official letter 12 months before their staging date.
But on 1 October, so-called “instant pension duties†took effect, and no more staging dates are being issued. Instead, anyone who starts up a new business or takes on a nanny/carer etc will have a legal duty to put an eligible employee straight into a workplace pension as soon as they employ him or her. In other words, they will have to provide a “staff pension plan†right from the start.
This will be a daunting prospect for many. However, the Pensions Regulator has launched an online set of information and tools for those employing staff for the first time.
There are a number of payroll companies out there offering to help people comply with their pension duties and deal with the admin, in return for a fee. Nannytax is one such firm – it describes itself as the UK’s leading nanny payroll provider. A spokeswoman for the company says its employer clients have reacted in different ways to being brought into the new pensions regime. While some see this as another cost they have to shell out for, others view it as “a really good thing†that their nanny is being encouraged to save for their retirement in this way.
One thing that’s not clear is what impact next year’s increase to pension contributions (see below) will have. Elliott Silk at investment company Sanlam UK says: “The rise from 2% to 5% coming into force in April 2018 will be a steep one felt by workers all across the country – the government, employers and wider industry need to prepare those who are likely to be affected by the increase, otherwise many people will be in for a big shock when they check their pay packet in April. We are encouraging employers to get the message out there early and provide financial education to their staff, highlighting the importance of saving and thinking beyond the minimum.â€
What exactly will it cost you?
So, if you employ a nanny or personal care assistant, how much might you – and they – have to pay into their pension? The answer is potentially quite a lot. By 2019-20 it could be £500-£600 a year each.
Under automatic enrolment, the total minimum amount paid in is currently 2% of qualifying earnings – typically made up of 0.8% from the worker, 1% from their employer and 0.2% in tax relief from the government.
However, in April next year this will rise to 5% (typically 2.4% from the worker, 2% from their employer and 0.6% in tax relief); and in April 2019 the total minimum contribution will ratchet upwards again to 8% – typically 4% from the worker, 3% from their employer and 1% in tax relief.
Just to complicate matters further, these percentages don’t apply to all of an individual worker’s salary, only to their “qualifying earningsâ€. This is what they earn over a minimum amount, currently £5,876 a year, and up to a maximum amount, currently £45,000 a year.
Let’s take the example of a nanny on a net wage of £350 a week. This translates into a gross wage (ie, before deductions) of £21,932 a year. According to Nannytax, which crunched the numbers for us, the employer contribution would be £160 a year (£3.09 a week), while the nanny’s would be £128 a year (£2.47 a week).
But these contributions will leap to £321 (£6.18 a week) and £385 (£7.42 a week) respectively in April next year; and from April 2019 onwards the employer will be coughing up £482 a year (£9.27 a week), while the nanny hands over £642 a year (£12.36 a week). Though don’t forget that the tax relief will also increase, too.
Nannytax points out that the lower earnings threshold changes at the start of every tax year, and we don’t yet know what it will be in April 2018 and April 2019, so it has to use the current £5,876 figure for the calculations. There is a calculator on the firm’s website that people employing a nanny can use to work out their pension costs.

‘Kinship carers’ denied thousands of pounds over two-child cap
Carers who voluntarily look after younger relatives to stop them being taken into care are being denied thousands of pounds in welfare entitlements as a result of the two-child benefit cap, despite government promises to exempt them.
Campaigners have called on ministers to change rules whereby kinship carers who act as guardians for at least two children are refused child tax credits and maternity grants when they decide to have a child of their own.
Ministers promised kinship carers a year ago they would not be subject to the two-child policy after a defeat over the issue in the House of Lords. However, it has emerged that the exemption only applies to carers who have birth children first and then become guardian to a third child – not the other way around.
Although in such cases the third child is the carer’s first birth child, officials have blocked child tax credit payments worth £2,780 a year because the claimant is considered to have breached the two-child limit that came into force in April.
Melanie Onn, Labour MP for Great Grimsby, said it was unjust that kinship carers who had made great personal sacrifices to care for relatives – and saved the state hundreds of thousands of pounds in fostering costs – were refused financial support.
“It’s unfair for people who have given up large parts of their life to take care of their close family. They do that with commitment and love, and without regret. To see them having children of their own and then having state support denied seems so incredibly unfair.â€
Onn has raised the case of a constituent, Alyssa Vessey, 22, of Grimsby, who was 18 when she gave up college to formally care for her three younger siblings following the sudden death of their mother four years ago.
Vessey was told that her application for child tax credits and a £500 Sure Start maternity grant before the birth of her baby this summer was refused because she had fallen foul of the two-child rule. She appealed twice but was turned down both times. Her son is now three months old.
She told the Guardian: “It’s unfair. They are saying if you take on children we won’t give you any money if you have a family of your own. People who save the government thousands by caring for children should get money and support when they have a family of their own.â€
The Department for Work and Pensions stood by the decision to deny child tax credits to carers like Vessey, saying it ensured fairness between claimants and taxpayers who support themselves solely through work.
A spokesman said: “We know some parents and carers are not in the position where their decision rests solely on whether they can afford a third child, and that’s why we have many exemptions in place. We continue to pay child benefit for all children in a household.â€
The two-child limit was introduced by the former work and pensions secretary, Iain Duncan Smith, two years ago on the grounds that it would force parents to “take responsibility†for their choices and teach them that “children cost moneyâ€.
Since April, as a result of the policy, families that have a third or subsequent child will no longer be able to claim child tax credits for this child or any future children. Tax credits are intended to help with the costs of bringing up a child.
The government expects to save more than £1bn annually by 2021 through the two-child cap, although charities estimate it will trigger a 10% rise in child poverty over the same period as affected families stand to lose nearly £2,800 a year.
Ministers, who had previously lauded kinship carers as “unsung heroesâ€, eventually agreed to exempt them from the two-child cap last year after a defeat in the Lords during the passage of the welfare reform and work bill. Opposition peers had argued that failure to exempt would deter potential carers from coming forward.
It has emerged that the government was warned about the anomaly affecting carers in Vessey’s situation by the Kinship Care Alliance last November in a formal consultation response, but this appears to have been ignored by officials.
Cathy Ashley, chief executive of the Family Rights Group charity, said: “It is particularly pernicious that this anomaly impacts on those who have gone the extra mile in caring for their younger siblings, often from a very young age.
“We did bring this to the attention of the government before the policy was introduced. However, we trust that its implementation is oversight and is urgently corrected by ministers.â€
Children move into kinship care for a variety of reasons, including parental death, neglect or abuse, parental illness, addiction, and imprisonment. An estimated 200,000 children in the UK are raised by kinship carers, saving the taxpayer billions of pounds.
Alyssa Vessey: teenage carer
When her mother died suddenly four years ago, Alyssa Vessey was a Grimsby teenager training to become a hairdresser. Just days later she was asked whether she would be prepared to look after her three younger siblings – become, in effect, their replacement mother.
She agreed willingly: “We went to social services and my family said to me ‘we’d understand if you didn’t want to take them on’. But my brother and sisters would have gone into care if I didn’t step up and bring them up; they’d be in the care system.â€
Becoming a kinship carer aged 18 was, she says, the hardest thing she’d ever done. “I had to do everything, waking them up in the morning and making sure they got breakfast, making sure they got to school, doing the tea when they got back, and making sure they did their homework.
“I was there for every parents’ evening, every GCSE meeting. I did everything to make sure the children do well in life.â€
Vessey says she had to give up her social life, and she lost friends as a result. Money was always tight as she adjusted to her new role. She got a job at Primark to help make ends meet and put a bit put aside to take her siblings to Lincoln on a rare holiday.
She is proud that this year the eldest of her three siblings, Keeley, went to university, the first in their family to do so. “I was determined that they had to make my mum proud, get the best grades they can. My mum always said she wanted the best for us all, to take every opportunity.â€
This summer Vessey and her partner, Adam, celebrated the birth of their own child, Joey. They have had to cut back hard after being informed that Joey did not qualify for tax credits or a Sure Start maternity grant because they had breached the two-child limit.
She said: “I think [the two-child rule] will put some potential carers off because not a lot of people out there know that when they take on children with guardianship they are not going to get any money for their own children. It’s going to be a lot tighter for them, but nobody knows about that.â€

Sign up to our e-newsletter
[mc4wp_form id=”16434″]

John’s Campaign
When someone with dementia is hospitalized, the medical staff should do all within their power to make access easy for family carers and utilise their expert knowledge and their love. The principles of John’s Campaign are applicable everywhere when a person with dementia cannot live in their own home. Whether someone with dementia is living in a mental health unit, a nursing home, a rehabilitation unit, supported housing or a care home, their families must be welcome to support them as often as they are able. Families are more than “visitors” to a person with dementia; they are an integral part of that persons life and identity and often their last, best means of connection with the world.
More recently, AgeUK have been taking an increasingly active role in the campaign’s promotion and implementation. They have produced an implementation guide and chair an advisory group of interested charities. For more information (email addresses and who to talk to), see our contact page.
Another organization that has had great influence on the campaign and its success is the Alzheimer’s Society. We were particularly inspired to take action by statistics in their 2009 report Counting the Cost: caring for people with dementia on hospital wards:
-
Over a quarter of hospital beds in the UK are currently occupied by people with dementia
-
The average stay of a person with dementia is three weeks but it can be much longer if rehabilitation is a problem or there is no where suitable to go
-
One third of people with dementia who go into hospital for an unrelated condition NEVER return to their own homes
-
47% of people with dementia who go into hospital are physically less well when they leave than when they went in
-
54% of people with dementia who go into hospital are mentally less well when they leave than when they went in
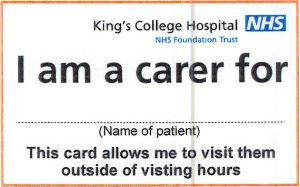
Kings College Hospital have signed up as members of John’s Campaign and are advertising across their wards. They have created a new carers passport card to help identify carers and allow them access to extended visiting hours and support.
Sign up for Advising Communities – Money Well Programme
They will be piloting a new approach which combines financial capability education, legal advice and 1:1 support. Participants in the project will benefit from small group training sessions as well as 1:1 advice and support over a 4-month period. They will be running the programme 3 times over the next year.
This project is aimed at providing participants with a holistic programme where they can deal with their immediate problems as well as building up their skills and resilience for the future with a heavy focus on financial capability.
Programme Schedule
As part of each programme the participant will attend 1 small group training session each month (4 in total). In addition, each participant will have regular 1:1 advice and support sessions with their caseworker, who will be a qualified legal adviser. 1:1 session’s will be organised directly with the participant’s caseworker who depending on capacity will try and be as flexible as possible to fit in with the participant’s schedule.
Start – October 2017. Finish – January 2018
Participation Requirements
This project is designed for clients with mental health conditions and low levels of wellbeing. In line with sector wide practice clients would fulfil this criterion if they self-identify as having a mental health condition or low levels of wellbeing (those with low levels of positivity and confidence and high levels of anxiety).
In addition, to benefit from this programme, clients must agree to complete all elements of the programme for the full 4-month period. This will include some evaluation exercises and questionnaires where results may be used anonymously in analysis. These will be used to ensure that participant feedback is used to shape the programme and also to demonstrate ‘what works’ about the project and the impact it has. Findings will be shared to improve learning in the sector and also to inform future projects. These questionnaires and exercises are designed to be user friendly and manageable. In addition, the participant’s caseworker will be available to assist in any way with completion of this.
Signing up or making a referral for this project
To sign up for this service please complete and send the attached programme sign up form.
Once completed please scan and send this to [email protected].
You could also post the completed sign up form by sending it to Jonakey Begum at the following address: Advising Communities, The Foundry, 17 Oval Way, London, SE11 5RR.
 If you are unable to email or post this to us, please call 020 3752 5494 for assistance in signing up.
The programme in more detail
The project is focused at combining 1:1 advice, support and small group training to improve participant’s financial capability.
Small group training sessions
The financial capability education element of this programme will take place in 4 small group training sessions. These sessions will be 2 hours long. All training sessions will include interactive activities, a chance for questions and discussions and also provided the participant with resources they can take away and use in the future. Once we have all sign up forms we will allocate participants into small groups and notify them of the sessions they should attend. We will take into account the participants time preferences as much as possible. Trainings session will typically have 6-10 participants attending.
Session will cover the following topics: attitudes to money and budgeting, maximising your income, banking skills, borrowing and saving, dealing with debt and welfare benefits.
1:1 sessions
Each participant will be assigned a caseworker for the duration of the programme. This person will be there main contact throughout and will also be the person holding regular 1:1 appointments. The participant’s caseworker is a qualified legal advice who is able to advise on all areas of social welfare law, such as housing, welfare benefits, debt and more.
At the first appointment the caseworker will work with the participant to put together an action plan of what they hope to achieve throughout the programme. Appointment can be used to get legal advice regarding any issues the participant may be having. This can involve the caseworker taking some actions on the participant’s behalf. These appointments can also be used to give the participant support but where this may not require legal advice. For example, the client may require help completing forms, writing letters or accessing digital services. In addition to this the client can use these appointments to reinforce their learning from the small group training sessions and apply this to their personal situation. For example, this may include creating and monitoring a personal budget, setting up a bank account or choosing financial products that suit their needs.
Appointments can take place at our Advice Hub or outreach locations. Depending on the participant’s availability appointments may also involve telephone or email advice and support.
Appointments will typical be 1-2 hours long depending on both the participants and adviser’s availability and the participant’s needs for that session.

Age-related dependency needs policy and long-term planning
These numbers represent a success story for modern medicine, public health and broader societal and economic conditions. Though there are major inequalities in healthy life expectancy at 65, and living with an increasing number of long-term conditions is becoming the norm for many older people, most reach their mid-70s without those conditions being life limiting or causing impairments in essential activities of daily living. Levels of self-reported wellbeing remain high well into older age.
This is positive news, and while we should avoid the ageist language of catastrophe – ‘grey tsunami’, ‘ticking demographic time bomb’, etc – we mustn’t duck the reality of planning future health provision and services to meet the needs of this ageing population. If we live long enough, most of us will need care and support in some form.
A rapid rise in the overall numbers living with dementia and frailty – when people live with lower reserve and resilience – is inevitable. Against this backdrop, there’s considerable interest in whether people who live longer will spend more years in a state of poor health or dependence, or whether so-called ‘compression of morbidity’ into the last phase of life is possible.
A recent Lancet paper gives an interesting perspective. Researchers looked at elements of dependency including continence, cognition and self-reported activities of daily living in two cohorts of people aged over 65 – one cohort recruited in 1991 and the other in 2011.
The bottom line finding from this research is that the men and women studied in 2011 were living, on average, an additional 2.4 and 3 years respectively with substantial care needs. Even with a radical shift towards healthy active ageing, it’s unlikely that a hypothetical 2031 cohort would show anything but an increase in the total number of older people living with dependency.
What are the implications of this for public policy? The study found that a smaller proportion of the 2011 cohort were in long-term residential care, despite the greater years lived with dependency. Some people have care needs so high that 24 hour residential support is necessary. The paper’s authors suggested that perhaps an increase in care home capacity would be required to match the increase in population dependency. Though this expansion might not be necessary if we invested in alternative kinds of support.
Currently, most support comes from informal family caregivers. Of six million people in the UK caring for an elderly relative, around two million are themselves aged over 65 and half a million are over 80. Many of these carers have their own health concerns that may be adversely affected by their caring role and few receive statutory help, despite government rhetoric about providing more support. There have been some aspirations in government policy and legislation around carer support, but funding hasn’t been made available to support it. The House of Lords Ready for ageing?report suggested that within the next decade, demographic demand for unpaid care will outstrip supply. What are we doing about it?
There is a need for more age-friendly housing and to provide more support in people’s homes. Yet we have failed to invest in the former and sustained funding cuts mean that last year 400,000 fewer people over 65 were in receipt of social care than in 2010. There is also a crisis in the health and social care workforce, compounded by the impact of Brexit on recruitment and retention, and of austerity on wages and morale.
Sadly, from Lord Sutherland’s Royal Commission on Long Term Care through the present day, we have had report after report – including one from the Barker Commission – all ducked by government of the day. In 2011, the Dilnot Commission on long-term care funding pointed out that social care is the one public service where risk isn’t shared and where some people will be hit for huge personal costs. As Dilnot pointed out in his response to the Lancet paper, there is no real appetite in the private insurance market for long-term care insurance.
We need the kind of public–personal partnership the Dilnot and Barker commissions recommended, but the febrile reaction to the Conservative manifesto promise to use the value of people’s estates to pay for their care – immediately branded a ‘dementia tax’ – or to Labour’s 2010 so-called ‘death tax’ shows how far we are from a mature public debate on social care funding.
Of course, we could aim to reduce some late-life dependency by investing in prevention and wellbeing: through exercise, reducing social isolation, preventing or delaying long-term conditions, or through secondary prevention – by helping people to live better with those conditions – we might reduce some of the need for care. Yet, the policy response to date has been to cut public health funding and the proportion of NHS funds going to primary care.
We could do far more to help older people recovering from episodes of illness or injury to regain their independence through investing in intermediate care rehabilitation or reablement and so reduce their reliance on formal or informal care. In reality, we only have around half the beds and places we need currently to do this, with capacity falling and response times increasing.
A final, intriguing suggestion to me from Professor Clive Bowman (an honorary visiting professor at the School of Health Sciences – City, University of London) was that we should set up a public health observatory of age-related dependence, its prevalence and duration to be tracked over time which could then be used to inform this crucial area of public policy.
The findings from the Lancet paper pinpoint the urgency with which we need to tackle the demographic challenge of age-related dependency. But is anyone listening?
