Latest News
Regular alcohol consumption could cut diabetes risk, study finds
Regularly drinking a moderate amount of certain alcoholic drinks could reduce a person’s chances of developing diabetes, according to a study.
Consuming alcohol three or four days a week was associated with a reduced risk of developing diabetes – a 27% reduction in men and a 32% reduction in women – compared with abstaining, scientists found.
Wine was considered particularly beneficial, probably because it has chemical compounds that improve blood sugar balance, researchers in Denmark found.
Gin could have the opposite effect, along with other spirits, increasing women’s chances of getting diabetes by 83%.
Experts said the findings, published in the journal Diabetologia, should not be seen as a green light to drink more than existing NHS guidelines suggest.
The authors of the research, led by Prof Janne Tolstrup from the University of Southern Denmark, wrote: “Our findings suggest that alcohol drinking frequency is associated with the risk of diabetes and that consumption of alcohol over three to four weekdays is associated with the lowest risks of diabetes, even after taking average weekly alcohol consumption into account.â€
In the past, studies have suggested that light to moderate drinking can reduce the risk of developing diabetes but there has been no research into the frequency of alcohol consumption.
Scientists studied data on 70,551 men and women who took part in a Danish survey. Respondents were quizzed about their drinking habits and monitored for five years.
Afterwards, participants were followed up and 859 men and 887 women had developed diabetes. The investigation did not distinguish between the two forms of diabetes, type 1 and the much more common type 2.
For both genders, seven glasses of wine a week lowered the risk of diabetes by 25% to 30% compared with having less than one glass.
Drinking beer seemed to affect men and women differently. Men who drank one to six glasses of beer a week saw their chances of getting diabetes lowered by 21%, compared with men who drank less than one a week. There was no impact on women’s risk.
Dr Emily Burns, the head of research communications at Diabetes UK, said: “While these findings are interesting, we wouldn’t recommend people see them as a green light to drink in excess of the existing NHS guidelines, especially as the impact of regular alcohol consumption on the risk of type 2 will be different from one person to the next.â€
Guidelines suggest that men and women should drink no more than 14 units of alcohol a week. That equates to about six pints of beer. It should be consumed over the course of three days or more, with some days of abstinence.
Burns said: “Type 2 diabetes is a serious condition, and around three in five cases can be prevented or delayed by eating healthily, moving more and losing weight if you’re overweight. If you’re worried about your risk of developing the condition, we’d advise you to speak to a healthcare professional.â€

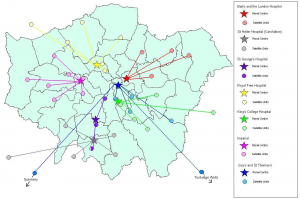
London Clinical Senate’s Patient and Public Voice (PPV) Group Recruitment
The London Clinical Senate provides independent advice to commissioners and other bodies, supporting them to make the best decisions about healthcare for people in London. The role of the Clinical Senate’s PPV Group is to act as the ‘voice’ of patients, carers and the public. Its views inform the advice given by the Clinical Senate.
As a PPV member, you will represent patients and carers who use London’s health services. You will also use your knowledge and experience to improve the quality of healthcare and to challenge the thinking of healthcare professionals where necessary.
Further information about the role and how to apply can be found in the Application Information Pack and also on http://www.londonsenate.nhs.uk/patient-public-voice/ppv-recruitment-2017/ . The application deadline is 8 September 2017.
Please direct any further queries to [email protected]Â or Sue Dutch (0113 80 70443).
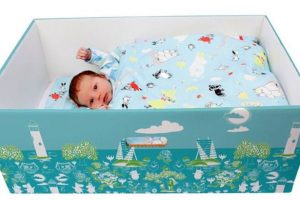
SLaM launches first mental health Baby Box programme in south London
As part of Baby Box University, an online resource to help with pregnancy and parenting, families will be able to access information from Maudsley clinicians on mental health issues, such as anxiety, postnatal depression and bonding with baby.
Parents attending South London and Maudsley’s Talking Therapies Southwark IAPT service will be offered a free Baby Box to provide a safe space for baby to sleep.
At a launch event in Bermondsey Central Hall, London, Senior Cognitive Behavioural Psychotherapist and Joint Perinatal Lead for Talking Therapies Southwark Katina Thomas, said:
“One in 10 women experience mental health distress during the perinatal period therefore it is important to help these women and their families to access support. We work closely with King’s College Hospital and Guys and St Thomas’s Hospital maternity services, to provide an effective service for those parents who are experiencing mental health difficulties during this time.
“The Baby Box scheme with its educational platform is an innovative way in which to incorporate maternity and mental health care to our clients. We are very excited to be launching the scheme and look forward to the therapeutic benefits it will bring. â€
Martha, mum to Ezra age 6 and nine-month old Olivia-Rose added:
“I felt low when I was on my own at home with my first baby. With my second I’ve been using Talking Therapies Southwark services and it is a therapy – you talk and they listen. The Baby Box programme will be a great addition to the support and help available.â€
Baby Box Co. Chief Executive Jennifer Clary, which is supplying the Baby Boxes and Baby Box University memberships for participating parents said,
“We are delighted to continue the expansion of the Baby Box and Baby Box University programme within the NHS in London.â€
The Baby Box tradition originates from Finland and has been credited with reducing the rate of sudden infant death in the country from 65 infant deaths per 1,000 births in 1938 to 2.26 per 1,000 births in 2015. The UK has some of the highest rates of infant mortality in Europe, ranking 22nd out of the 50 European countries with 4.19 deaths per 1,000 births.
Half of children needing summer food bank support are in primary school
The UK’s biggest food bank network, the Trussell Trust, has revealed that 67,500 three-day emergency food packages went to children in July and August 2016 – 4,000 more than in the preceding two months.
The research shows that 47% of the children receiving supplies from food banks were aged 5-11, while 27% were under five and a fifth were aged 12-16.
Samantha Stapley, operations manager for England at the Trussell Trust, said the statistics highlighted “just how close to crisis many families areâ€.
She added: “As a nation, we also must address the reasons why families with children are referred to food banks in the first place. We welcome the government’s decision to maintain free school lunches for children during term time – the next step must be to help families during the holidays.â€
The Rt Rev the Lord Bishop of Truro, Tim Thornton, described the figures as shocking, adding: “That so many primary-age children are going without food in our country is of great concern.
“It is very good that the community wants to help and work with those less fortunate and that is a key part of the gospel values. It is, however, also important that we keep trying to understand the deeper reasons why this situation is as it is.â€
Stapley said food banks were doing more than ever before, but voluntary organisations “alone cannot stop primary school children facing hungerâ€. She called for a long-term coordinated solution to help keep families from “falling into crisisâ€.
The Trussell Trust said the proportion of primary school children helped by food banks was consistently high all year round, with 46% of the children referred in the year to March aged between five and 11.
The charity said it was offering extra help to families this summer, with additional services including a holiday club. Trained volunteers will talk to parents to understand why they are struggling and offer support.
Imran Hussain, director of policy, rights and advocacy at Child Poverty Action Group, described the data as incredibly worrying but not surprising. “Children are twice as likely to be poor than pensioners,†he said. “The poverty rate for children is 30% and for pensioners it’s 16%. The trajectory for child poverty is that it will hit 5 million by 2022.â€
Hussain added that wage stagnation and cuts to benefits were behind the stark figures. “We need to make sure a basic level of benefits is there to meet the needs of children – that is a chronic issue that needs tackling,†he said.
“We know summer is tough for families, particularly those with young children, and it can be difficult to get time off or afford childcare to pay for it … you hear anecdotally that some parents leave jobs every summer to look after their kids.â€
A government spokesman said: “Record numbers of people are now in work and we’re helping millions of households meet the everyday cost of living and keep more of what they earn.
“We’ve doubled free childcare to help parents into work, and continue to spend over £90bn a year on support for those who need it, including those who are bringing up a family or on a low income.
“Budgeting advice and benefit advances are also available for anyone who needs more help.â€
If your family are struggling, Southwark Carers are a registered food bank voucher provider, please call in to the office to discuss.

UK shops to fall quiet to help people with autism
Shops across the UK will fall quiet later this year as part of a project to raise awareness of autism.
The “Autism Hour†event has been organised by the National Autistic Society to help draw attention to the difficulties that people with autism can face in noisy environments.
In the first week of October, businesses will turn down music, reduce tannoy announcements and dim lights to help create a calming and less daunting environment.
Shop workers will also be given information about autism and how they can support autistic people.
A number of major retailers have already signed up to the initiative, including Clarks and Toys R Us.
Research by the National Autistic Society shows 79 per cent of autistic people feel socially isolated and 64 per cent avoid going to the shops. A further 28 per cent have been asked to leave a public place because of something associated with their autism, while 16 per cent of people with autism feel the wider public understands them.
More than one in 100 people in the UK are on the autistic spectrum.
Mark Lever, Chief Executive of the National Autistic Society, said: “We’re delighted by the response to Autism Hour so far. These simple steps will lead to a more autism-friendly world.â€
Families of people with autism welcomed the campaign. Natasha Lee, who lives in north Wales and has three autistic sons, told The Sunday Times: “The only way I can describe the feeling when the public mistake your children’s behaviour during a meltdown, is gut-wrenching.
“When people are staring at and judging your child for being naughty and you know that really they are in incomprehensible pain, experiencing noise as loud as a blaring concert and light so bright it’s the equivalent of shining a torch in their eyes, it just makes you feel helpless.
“If Autism Hour can successfully improve understanding and support of my children’s needs, I would feel an overwhelming amount of hope.â€
Matt Davis, whose nine-year-old son Isaac is autistic, said: “Noise, lighting and crowds are all triggers for Isaac, so either we avoid shops altogether or we have to put in a great deal of preparation to ensure my son doesn’t become overwhelmed.â€

Innovative digital therapy for paranoia
Paranoid thoughts are one of the most common symptoms of severe mental health problems, and are associated with significant distress and disability. But pharmacological and psychological treatments have limited effectiveness, so innovation is urgently needed.
SlowMo is the culmination of three decades of research, led by Professor Philippa Garety, Clinical Director and Joint Lead for the King’s Health Partners Psychosis Clinical Academic Group (CAG). This work initially found that fast thinking habits contribute to paranoia, and a talking therapy promoting slower thinking showed promise in helping people cope with their concerns.
SlowMo is an easy-to-use, memorable and enjoyable digital therapy, a development led by Dr Amy Hardy of King’s College London and South London and Maudsley, in collaboration with service users, clinicians, inclusive healthcare designers and technologists.
SlowMo works by supporting people to notice their upsetting worries and fast thinking habits, and then provides tips to help them slow down their thinking and cope with paranoia. It consists of eight face-to-face sessions with a therapist, assisted by a website with interactive stories and exercises. This synchronises with a mobile app for use outside sessions, extending the reach of therapy to people’s daily lives.
Initial feedback about SlowMo has been very positive, with people indicating it has helped them manage their fears and get more out of life.
The trial will determine whether SlowMo reduces paranoia, and if it works by improving slow thinking. 360 people with schizophrenia-spectrum diagnoses in total across three sites (120 from South London and Maudsley) will be randomly allocated to continue with their usual care, or receive SlowMo plus their usual care, and followed up over six months. If SlowMo is found to be effective, Professor Garety’s team plans to make it freely available in the NHS.
The King’s Health Partners Psychosis Clinical Academic Group brings together the largest group of psychosis expert clinicians, researchers, academics and clinical staff in the world.
For more information about the trial visit the SloMo website.
The trial team, funded jointly by the Medical Research Council (MRC) and National Institute for Health Research (NIHR), will be recruiting participants from the Psychosis CAG at the Trust over the next two years.

Nursing shortages fuelling delayed discharge from hospital
There is no doubt that delays in arranging follow-on social care are causing more older people to be stranded in hospital. But a new analysis of the problem says shortage of district nurses is at least as big a factor.
The number of district nurses in the UK has plummeted by 44% since 2010 when counted as full-time jobs, according to the analysis of NHS data by consultancy Christie & Co (pdf).
The trend is described as a “key trigger†of hospital admissions of older people and of subsequent delayed discharge. District and other community nurses play a crucial role in treating people in their own homes or in care homes when they might otherwise be referred to hospital.
Since 2008, numbers of people aged 60 and over admitted to hospital have soared 65%, the analysis finds.
Michael Hodges, head of care consultancy at Christie & Co, says ministers are missing the bigger, more complex picture behind delayed discharge by focusing narrowly on blockages in the social care system.
“We need to take a much more rounded view of the whole health and social care system,†he says, “including workforce planning for essential roles like district and community nurses and a proper assessment of what more social care providers could offer to ease pressure on hospitals.â€
According to a breakdown of delayed discharge figures by Christie & Co, some of the areas said by the NHS to have the worst problems have ample capacity in local care homes to accept older people from hospital for short-term “reablementâ€.
Homes in Birmingham, which is said to have the biggest delayed discharge challenge, are shown to be operating at only 77.5% capacity. Those in Hampshire, which is said to have the second most severe problem measured by number of days of discharge delays, are running at 84.2%.
“There are great opportunities – and not just for a quick fix,†says Hodges. “I really hope that somehow the politicians look at it properly and strategically for the long term.â€
The analysis includes a survey of fees paid to care homes for state-funded residents by 123 English councils, four in five of the total, plus figures for fees charged by more than 200 care providers.
On average, “base†fees offered by councils are shown to have increased by 3%-4% this year. But providers have been able to negotiate better terms for care of older people, with an average uplift of 5.2%.
By contrast, fees for “specialist†care such as learning disability or low-secure accommodation have risen by only 1.9% on average – the second successive year to show such disparity.
Hodges says providers are starting to think twice about investment in specialist care and suggests policymakers need “urgently†to look at funding for this part of the social care sector.
The survey confirms a continuing trend of care home providers squeezing self-funding residents, with an average fee increase of 6.3% for private payers and as big a rise as 9.8% in one case.

Dozens of leading charities face insolvency after Government demands back pay for night-time carers
Vulnerable people with learning difficulties face losing “vital†care as a result of the bills, charities have warned, with around 5,500 supported by Mencap alone set to be “majorly impactedâ€, while some may end up losing that support all together.
Under guidance issued by the Government in 1999, when the minimum wage was introduced, disability charities, which sent a carer overnight to look after someone with learning difficulties, were required to pay a flat rate “on call†allowance of £25 or £35 to cover the period when they were asleep.
But, following two tribunal cases in 2015 and last year, the Department for Business, Energy and Industrial Strategy (BEIS) changed the guidance in October to state that these organisations must now pay the minimum wage throughout the shift, meaning overnight carers would earn £60 for eight hours of sleep.
Mencap and other charities and companies are now warning that they cannot afford the huge and unexpected additional sums being demanded by HM Revenue & Customs (HMRC), even though they believe their staff should get the higher pay levels demanded by the business department.
Derek Lewis, chairman of the Royal Mencap Society, said “sleep-insâ€, which are widely used in the sector, rarely see the carer disturbed during the night, citing research showing that 99.7 per cent of them slept peacefully.
“Sleep-ins are widely used in the learning disability sector to provide care for some of our most vulnerable adults, in their own homes in the communities they live in,†he said.
“The carer is only there ‘just in case’ to provide safety and reassurance and is rarely disturbed. Recent research which looked at the last three years showed that 99.7 per cent of carers slept peacefully.
“The unintended consequences have been disastrous as HMRC have begun enforcement action demanding six years’ back pay. Estimates of the costs to the Learning Disability sector are in the region of £400m and Royal Mencap Society will be severely affected.â€
Mr Lewis added that “high politics, Brexit or the Parliamentary Recess†appeared to be “getting in the way†of talks between charities and the Government about the issue.
The national minimum wage for those aged 25 and over is £7.50 an hour, which will increase to £9 by 2020.
About 178,000 people with learning difficulties may lose their assistance at home because of changes to pay rates for 24-hour care, with one large provider ordered to come up with six years’ back pay by September, said Mr Lewis.
He added: “For many smaller care providers across the country, the financial impact will be devastating. The resulting multiple insolvencies will be more serious than Southern Cross because there will be no alternative providers available, as local authorities are already finding. We know that the Care Quality Commission is very concerned.”
Jan Tregelles, chief executive of Royal Mencap Society, said: “We all recognise that our social care colleagues do some outstanding work and are some of the lowest paid, but we cannot pay them if we do not have the money and we only receive money from government sources.
“For someone with serious learning disabilities, having someone stay overnight ‘at home’ makes the vital difference between ‘living a life’ and spending the rest of their life in a hospital setting.

Services ‘too often’ failing to apply Mental Capacity Act properly
Vulnerable adults are too often being let down by social workers and care providers failing to follow the Mental Capacity Act properly, a report has warned.
The Local Government and Social Care Ombudsman’s review found one in five social care complaints made to the service last year concerned mental capacity or deprivation of liberty cases. More than two-thirds of these complaints were upheld, compared to 53% of all complaints across social care.
The watchdog published details of seven cases it said highlighted common issues in the way the MCA and DoLS are applied. These included delays carrying out assessments, poor best interests decision-making, and a failure of services to involve family in the process.
In one case flagged by the ombudsman, a stroke victim was placed in a care home against his will after social workers made assumptions about his capacity without properly assessing it. He was later found to have the capacity to decide where to live.
‘Delays in authorisations’
The report also highlighted significant problems with the DoLS, which included delays in councils and care providers applying for a DoLS authorisation.
In one case, a care home took six months to apply for a DoLS order for one of its residents who had dementia. The council involved also failed to inform the man’s wife of the order.
The report acknowledged that councils had struggled to keep up with the rise in DoLS applications following the landmark Cheshire West ruling, which effectively lowered the threshold for cases requiring an authorisation, leading to a ten-fold increase.
However, it said that the ombudsman’s investigations showed some councils and care providers did not properly understand the decision-making process.
Michael King, the local government and social care ombudsman, said the people these measures were designed to protect were “all too often†let down by poor practice.
“While I appreciate the complex emotional and practical decisions social workers need to make, the people they look after are still entitled to be treated fairly, and have their assessments undertaken correctly and in a timely manner,†he said.
‘Singled out’
Rob Mitchell and Mark Harvey, co-chairs of the adults’ principal social worker network, said: “We have not seen the report in detail so we are unsure whether the 69% of upheld complaints are wholly in response to the actions of social workers, or whether they are concerns relating to the actions of other agencies, including the NHS and care providers.
“However, it is wrong to single out social workers as they are not the only profession who assess capacity. While we know nationally social workers are leading the response in ensuring that mental capacity is embedded, others are taking an increasing role. This is especially true in places such as hospitals, where the lack of knowledge and application of the MCA and Code of Practice is particularly concerning.â€
They added: “For those who need or look to social work for a professional, person-centred and high quality response in relation to Mental Capacity Act practice, we are confident that in the majority of cases that is exactly what they will receive. Despite the worrying evidence in this report it is key to remember these are small numbers compared to those undertaken by social workers everyday across the county.
“It is also important to understand the level of pressure and expectations being placed on adult social work today. Expectations to deal with system failures, poor local commissioning arrangements and lack of available care, on top of increasing referrals, are often diverting social workers from these core practice areas. Social workers themselves though need to ensure they prioritise their response to citizens and ensure good practice in these areas remain a key focus and area of pride in our roles.â€
‘Unprecedented levels’
The report also included two examples of good practice, which showed where councils and care providers had followed the correct procedures.
Margaret Willcox, president of the Association of Directors of Adult Social Services, said: “We are always disappointed to hear of poor practice and one instance is one too many. We are not complacent but are aware there is also good practice, as evidenced in the report.
“The report recognises that DoLs applications in England have soared to unprecedented levels in the past two years, leading to huge delays in processing. We hope the Law Commission’s plans to introduce new, more efficient DoLS legislation helps to address this and alleviate any further concerns and anxiety for families and individuals involved.â€
CQC warns mental health sector is ‘at a crossroads’ – some services responding positively to unprecedented challenges but others must move away from out-dated care that leaves people ‘helpless and powerless’
Inspectors found many examples of excellent care – but they also found too much poor care and far too much variation in both quality and access across different services. This is particularly concerning given the increasing demand for mental health services, meaning that more people risk receiving care that is not good enough – or no care at all.
By 31 May 2017, 68% of core services provided by NHS trusts and 72% of independent mental health locations were rated as good; with 6% of NHS and 3% of independent core services rated as outstanding. Of the 22 NHS trusts originally rated as inadequate or requires improvement that we have re-inspected, 16 achieved an improved overall rating. And nearly all NHS and independent services were rated as good or outstanding for having caring and compassionate staff (NHS: 88% good, 9% outstanding; independent: 93% good, 5% outstanding).
However, the report identifies several areas of concern:, physical environments not designed to keep people safe, care that is over-restrictive and institutional in nature, and poor recording and sharing of information that undermines the efforts of staff to work together to make sure that people get the right care at the right time.
Dr Paul Lelliott, Deputy Chief Inspector of Hospitals (Lead for Mental Health) at the Care Quality Commission said: “More than ever before, people are being encouraged to talk openly about mental health conditions and to share their experiences – and more people than ever are receiving treatment and care for mental health conditions, in part due to a reduction in the stigma associated with mental ill health. But this vital work must be supported by services that give people the help they need, when they need it.
“The mental health sector is at a crossroads. The Five Year Forward View for Mental Health, published last year, along with the newly introduced waiting time standards, point the way to a future where people have easy access to high quality care close to home and are able to exercise choice. To achieve this vision, the sector must overcome an unprecedented set of challenges – high demand, workforce shortages, unsuitable buildings and poor clinical information systems.
“Some services remain rooted in the past – providing care that is over-restrictive and that is not tailored to each person’s individual needs. This can leave people feeling helpless and powerless. But the best services are looking to the future by working in partnership with the people whose care they deliver, empowering their staff and looking for opportunities to work with other parts of the health and care system.
“These outstanding mental health services provide world-class care, whether in hospital or in the community; the challenge is how to ensure that everyone, no matter where they live or who they are, has access to services of this quality. The good news is that mental health services in England have the raw material to achieve great things.
“We have rated almost every service as good or outstanding for caring – ratings that were informed by our own observations and with interviews with many thousands of staff and patients.
“Those who deliver and commission care must learn from the services that are getting it right. And we will continue to highlight good practice, drive improvement and act on behalf of people to ensure that everyone gets the help they need when they need it.”
Inspectors found that some types of service shone out: community services for people with a learning disability or autism performed particularly well; with 80% rated good and 9% as outstanding. In these services, inspectors found that staff were skilled and appropriately trained, patients were involved in planning their care, and there were systems in place to deal with urgent referrals.
However, looking across all care settings, the report identifies several areas of concern:
Restrictive practices. There are about 3,500 beds in locked mental health rehabilitation wards, with about two-thirds managed in the independent sector. These wards are often situated a long way from the patient’s home, meaning that people are isolated from their friends and families. Inspectors were concerned that some of these locked rehabilitation hospitals were in fact long stay wards that risk institutionalising patients, rather than a step on the road back to a more independent life in the person’s home community. Another area of concern was the great variation between wards in how frequently staff use physical restraint to manage challenging behaviour. CQC is further strengthening its assessment of how and how often services use physical restraint, and will be subjecting those services where staff frequently resort to restrictive interventions to much tougher scrutiny.
Safety. This was the area in which services were most likely to perform poorly, with 4% of NHS core services and 5% of independent mental health core services rated as inadequate for safety and only 59% and 61% respectively rated as good. On too many wards, the combination of a high number of detained patients who pose a risk to themselves and sometimes to others, old and unsuitable buildings, staff shortages and a lack of basic training, make it more likely that patients and staff are at risk of suffering harm.
Patient clinical information systems. Many clinical staff told inspectors that they had difficulty recording and retrieving information that was sometimes critical to patient care, and had to work with a confusing combination of electronic systems and paper. Ineffective clinical information systems can have a real impact on people – for example, crisis teams not being able to access records for patients taken to a health-based place of safety, which could prevent people getting the care they need at the time they need it most.
Underpinning all these concerns is the fact that mental health services are under significant and increasing pressure. National figures show a continuing decline in the number of mental health nurses (a 12% fall between January 2010 and January 2017), and the number of inpatient psychiatric beds reduced by 4% overall between 2014/15 and 2016/17. At the same time, the number of detentions under the Mental Health Act rose by 26% between 2012/13 and 2015/16.
Providers have tough decisions to make, and there are no easy answers. However, the decisions that are right for people are often those that are right for organisations too:
treating people as active participants in their own care promotes recovery and lessens dependence on services;
investing in better services locally prevents the need for costly out of area placements that risk isolating people from their family and friends; whether that is for an acute admission, or to a psychiatric intensive care unit or to a locked rehabilitation ward; and
investing in information technology that enables staff to enter and retrieve clinical information while on the move will reduce wasted staff time and make care safer.
Leadership that supports staff to work to their full potential not only increases the likelihood that people will receive good care but puts providers in a stronger position to face a future in which the scale of the challenge is unlikely to decrease.
Commissioners, too, have a responsibility to ensure that the services they are buying with public money are right for the people using them.
CQC will play its part by ensuring that everybody gets the care they need to recover – sharing best practice, driving improvement and taking action to protect people where necessary. To help do this, CQC will continue to work closely with experts in the field of mental health care to ensure that inspectors understand the latest thinking on what is a rapidly evolving area of policy and practice.
The best mental health services in England provide care in hospitals and round-the-clock care in the community that is world-class. The characteristics of outstanding providers – like Northumberland, Tyne and Wear NHS Foundation Trust and East London NHS Foundation Trust – are those that display clear leadership, both at a provider and ward level, that ensure their staff have the systems in place to enable them to do their jobs properly and that shape the care they deliver around the people who receive it.
#StateofMH
