Latest News
Social workers alert Hunt to dangers of mental health bed shortage
A group of approved mental health professionals has issued a direct plea to Jeremy Hunt to address failings in mental health provision it says are placing vulnerable patients and families at risk.
In a letter to the health secretary, the Yorkshire AMHP leads network warned a shortage of mental health beds meant some patients assessed as needing to be detained under the Mental Health Act for their own safety, or that of others, were being forced to wait days to get hospital care.
The group said some patients had been held in A&E departments, police stations or care homes until a bed became available, but others were left at home relying on families or friends to manage their “acute mental health crisisâ€.
“We are asking you to give the situation your immediate and highest priority before any more patients and their families have to experience this very distressing and potentially dangerous situation again,†the group’s letter said.
Andy Brammer, a member of the Yorkshire AMHP leads network, said the group raised its concerns with Hunt in March but had yet to receive a reply.
A Department of Health spokesperson said Hunt had sent a response to the group’s concerns on March 31. The spokesperson said the government was investing in mental health services to make sure the right support was in place.
Speaking to Community Care yesterday, Brammer said the issues raised in the letter remained “live†and AMHPs still often faced “significant delays†securing beds for people in crisis.
“There is a lot of consideration that goes into detaining someone under the Mental Health Act. It is a last resort. People being detained are often those at most risk to themselves or others, and in the greatest level of distress,†he said.
“To have that detention delayed for hours, or even days, just increases that level of distress for the person and their family. It’s very stressful for workers as well who are having to manage the situation.â€
Brammer added: “Previously AMHPs were waiting hours for beds to become available in virtually all circumstances. Then we saw it shifting to waiting 24 or 48 hours, and that tended to be with people who were in places like A&E – it wasn’t ideal but at least they were somewhere safe.
“We’re now looking at people being in their own homes and being left with a phone line for services. It’s an invidious position for everyone involved.â€
Ruth Allen, chief executive of the British Association of Social Workers, said the concerns raised by the Yorkshire AMHPs echoed those raised by practitioners in other parts of the country.
“The feedback we get from AMHPs is that the bed situation has not been resolved in most areas,†she said.
“The focus on improving mental health crisis services, through the government’s crisis care concordat policy, does not appear to have led to better preventative resources for people to avoid admissions or opened up pathways into beds when they are most needed.â€
Figures published last month revealed almost 6,000 mental health patients were sent out of their local areas for care last year due to no beds being available locally. This marked a rise of 40% over two years. NHS England has pledged to end inappropriate out-of-area admissions by 2021.
An investigation by Community Care and BBC News published in 2014 found seven suicides and one homicide had been linked to mental health bed shortages over the previous two years.
In December 2013, Nigel Meadows, senior coroner in Manchester, alerted Hunt and NHS England to problems with bed availability following the suicide of a patient who had been assessed as needing ‘urgent admission’ but faced an eight day wait for care.
A Department of Health spokesperson said: “We are clear that inpatient services should be available for all who need them. Decisions about bed numbers are based on a local assessment of need. We are making sure the right services can be put in place, with annual spending on mental health services increasing, now at more than £11 billion.
“In addition, getting community support right is vital, that’s why we are investing £400m a year by 2020 to expand the Crisis Resolution Home Treatment teams which will help open up in-patient beds.â€

Nominate someone for a Headway Award
Each finalist, chosen by a selection panel, will be invited along with a guest to a glittering luncheon at The Dorchester Hotel in London on Friday 8 December.
Do you know someone who has defied their brain injury to achieve a great milestone this year? Or perhaps you know someone that often goes above and beyond when caring for someone with a brain injury? Or maybe you know of a long-standing Headway volunteer who is overdue public recognition and thanks?
The categories this year are:
- Carer of the Year sponsored by SweetTree Home Care Services
- Alex Richardson Achiever of the Year sponsored by Slater & Gordon Lawyers
- Volunteer of the Year sponsored by Anthony Gold
- Stephen McAleese Outstanding Contribution to Headway Award sponsored by No5 Barristers Chambers
What we’re looking for
The more information we have about the person you are nominating, the better their chance of being shortlisted for a Headway Award!
- Share your passion! We don’t know the person you’re nominating, so don’t spare the details – or your feelings about how special they are!
- Give us details. How long have they been a volunteer? How much progress have they made since sustaining their injury? What have they sacrificed to care for someone?
- Set the scene. How did life change? What was life like before? Why does your nominee stand out from the crowd?
- More is more! Keep your information relevant and catchy, but don’t hold back. The more information we have, the better.
If you would like to nominate someone, please click the button:
Cambridge House Law Centre – Employment and Discrimination Advice
Advice is by appointment only and is available solely for people who live or work in the London Borough of Southwark.
The one off advice sessions are held on Tuesday afternoons from 14:00 with four appointment slots at each session.
How to book an appointment:
- Call in person and speak to the Law Centre receptionist;
- Telephone the Law Centre on 020 7358 7025
- Email the Law Centre receptionist: [email protected]
Session dates for 2017
Tuesday 18th July
Tuesday 1st August
Tuesday 15th August
Tuesday 29th August
Tuesday 12th September
Tuesday 26th September
Tuesday 10th October
Tuesday 24th October
Tuesday 7th November
Tuesday 21st November
Tuesday 5th December
Tuesday 19th December

Invisible heroes: On the frontline with the UK’s army of elderly carers
Elderly carers have expressed their “disgust†at being stripped of an “essential†benefit once they reach pension age and are calling on the Government to recognise their contribution to society – and the economy.
Carers in the UK can be eligible to receive £62.70 per week Carer’s Allowance if they look after somebody else for at least 35 hours per week.
Pensioners ineligible for benefit
However, while there is no upper age limit for claiming Carer’s Allowance, carers are not permitted to receive the full amount of both this and their state pension simultaneously as the two are classed as “overlapping benefitsâ€, the charity Carer’s UK has pointed out.
If a person is receiving Carer’s Allowance when they reach retirement age and their state pension is greater than this amount, then the benefit will be stopped. If their state pension is less than their Carer’s Allowance they can get the difference paid in Carer’s Allowance.
‘I turned 65 the day the letter came’
Colin, 66, lives in Herefordshire with his wife of 42 years, Heather, who has fibromyalgia, a long-term condition that causes pain all over the body.
The former RAF flight assistant, who asked that his full name not be published, was stunned to be informed that he would no longer receive his Carer’s Allowance when he reached retirement age.
“The day I turned 65 the letter came,†he says.
Heather, who is also 66, is reliant on Colin to do everything for her, from helping her to shower and cutting her toenails, to massaging her legs and administering medicine, as well as cooking, cleaning and taking her to medical appointments.
Taken for granted
But his contribution “taken for granted†by the Government, he says.
“I think it’s disgusting…I worked from 15 to 65 and I’m struggling financially,†he adds.
Money is tight – so much so that even purchasing the appropriate food for Heather (it’s essential that she maintains a healthy weight) is growing increasingly difficult.
The couple, who have three surviving adult children – their son died last year aged 37 – and five grandchildren, are struggling to scrape the money together to buy a reclining chair for Heather – her current one is on its last legs.
‘DWP didn’t want to know’
“[Carers are] saving the Government billions. That £63 a week can make a difference…I rang the DWP [and] they didn’t want to know,†Colin says.
Asked to describe his feelings about being refused Carer’s Allowance he hesitates. “I couldn’t. You couldn’t print it,†he explains.
Colin is one of countless carers up and down the country in this position.
Does anyone care?
“If everyone who was a carer took their partner or child to the local hospital and said, ‘Look after them for 24 hours, this country would stop,†he says.
What’s the solution? It’s simple, Colin says: “Money.†For pensioners like him, £62.70 per week would be a good start. But, he adds: “Nobody wants to know. Nobody cares.â€
Another male pensioner, who asked to be known only as David (not his real name), cared full time for his wife for 26 years until she passed away in 2012.
Saving the state a fortune
David’s wife Moira (also a pseudonym), suffered from severe rheumatoid arthritis over most of her body and lived with “terrible painâ€, though was an “inspiration†to her husband.
“I did get a little help [financially] until I received my pension, then that stopped,†says David.
“It’s damned unfair… you should get your pension and Carer’s Allowance. You’ve paid in and you’re saving the state an absolute fortune by being a fulltime carer.â€
No conscience
The couple, who lived together in Cornwall, celebrated their 50th wedding anniversary the year before Moira died.
David does not expect any praise for the care he gave Moira – “I loved my wife dearly,†he says – but he believes the Government is taking advantage of the huge number of “hidden†workers.
“Everybody in power knows what’s going on,†he says. “If they had any conscience at all they’d correct that anomaly.â€
£15bn contribution
Emily Holzhausen, director of policy at Carers UK, said: “Older carers make a huge contribution to our society estimated to be worth £15 billion a year, and those aged over 65 years old are now the fastest growing group of carers.
She added: “Sufficient and sustainable funding for health and care services is urgently needed to give older carers the support they need.
“The Government should also review how the contribution of older carers can be better recognised in the social security system.â€
The DWP said in a statement: “Carer’s make a huge contribution to society.
“Carer’s Allowance and State Pension are both designed to replace income and we pay the higher of the two amounts to carers of State Pension age.â€

Chickenpox jab offered on the High Street
Superdrug will be offering it at 58 of its specialist pharmacist stores at the cost of £130 for a two-dose course.
The vaccine is only available on the NHS for people at high risk of spreading the virus to those with weakened immune systems.
The NHS says a routine childhood chickenpox vaccine would raise the risk of more serious infections in adults.
Ninety per cent of people catch the chickenpox virus by the age of 15 and in most cases it is uncomfortable but leaves no lasting effects.
Symptoms include an itchy red rash of spots and blisters, and a fever, as well as tiredness, nausea, headache, muscle ache and loss of appetite.
People who catch the virus as a child normally become immune for life, although one in three adults can develop shingles.
Adults can still contract the virus but symptoms and possible complications are usually more serious, including the risk of pneumonia, hepatitis and encephalitis.
The NHS said a chickenpox vaccine is not offered as part of routine immunisations as it would leave unvaccinated children more susceptible to contracting the virus as an adult.
There could also be a significant increase in shingles cases as being exposed to infected children boosts immunity to this.
People have for some years been able to pay to get the vaccine from a variety of sources outside of the NHS such as travel clinics.
Dr Pixie McKenna, a TV doctor who advises Superdrug, said: “Chickenpox is often seen as a rite of passage in childhood resulting in anything from a very mild to a more serious infection in different people. Even in straightforward cases, spot picking can lead to long-term scarring which can linger long after the infection is gone.
“A chickenpox immunisation has been available for many years but not on the High Street until now. Having suffered from severe chicken pox at the age of 19, I would far rather have undergone the vaccine than be struck down with the infection!”
The vaccine will be available in 58 Superdrug stores, across the UK.
The store recommends two injections, four to eight weeks apart.
Chickenpox immunisation has been available in the US for children under 13 for 20 years and research by the Paediatric Infectious Diseases Society shows it has seen hospitalisations due to the disease fall by 93%.

How to Communicate When Your Elderly Parent Can No Longer Speak
On instinct, the husband decided he would do what he’d always done. He climbed into her bed with her and held her. He cuddled with her. He stroked her face and told her he loved her. He spent hours just snuggling and holding her.
Slowly, the wife responded. This once angry, difficult woman became easy for the staff to handle. She was, once again, friendly, cooperative and generally happy.
This particular story was recent, riveting and poignant. However, human touch has long been known to soothe a being who cannot communicate. Babies who live in orphanages where they are not held and cuddled often die. That need for human touch never goes away.
Many of us are coping with elders who can no longer communicate. Whether from a stroke, Alzheimer’s, Parkinson’s or for some other reason, they have lost their ability to talk or seemingly respond in any manner to their loved one’s efforts to communicate.
Caregivers want to communicate with them, but when they visit their elder and see them in this non-responsive mode, they tend to sit there uncomfortably watching the clock – putting in time, so to speak. There’s a feeling, for many of, “what’s the use?”
It’s said that hearing is the last sense to go. I feel, just from what I’ve seen and read, that the sense of touch is right up there with hearing. Between the two, it’s amazing what a caring person can do to help someone who seems lost to them.
We need to remember that someone who cannot talk is very vulnerable. She can’t say what feels good or what she doesn’t like. So, if you are using touch as a means to communicate, you need to be very tuned in to body language. The same goes for providing communication through hearing. Many times the two are connected. Watch the person’s body language carefully to see what you should continue, or what you should change.
If you are providing any type of hands-on care for a person in this condition, speak soothingly and continuously, about what you are doing. Say things like, “I’m going to rub lotion on your arm now. Does that feel good?” or “I’m going to brush your hair now. It will really look nice.”
If you are not providing necessary physical care, you can still do pleasant touch therapy, such as lotion or massage oil on the arms and legs, saying, “I’m putting some nice warm oil on your arm now. Does that feel good?” Just keep the talk soothing and the touch light. Make sure any ointment you use is warm, but not hot. Think of what you would like if the situation were reversed.
If you are mainly there to converse, or if your elder doesn’t seem to like too much touching, honor that. Perhaps you could hold his hand while you talk about familiar things such as family or events he would remember with pleasure. Gently hold his hand and perhaps lightly place your other hand on top. The idea is to connect in a pleasurable way.
Music and Reading Help Caregivers Communicate With Mute Seniors
Listening to music, if it’s the kind your elder likes, can be healing and powerful. I kept a CD player in my dad’s room. He loved big band music. I kept him supplied with new CDs that were easy to find online. He loved the music on his better days. He even would “direct” the orchestra, much to the puzzlement of strangers walking by his room and loving amusement of the nursing home staff. On days when he couldn’t respond, music would still play as he lay there. It seemed to help him relax.
Some people enjoy being read to. You could find your dad’s favorite books and read chapter by chapter, depending on his level of enjoyment. If he loves the Bible, you could read his favorite verses. Whether or not he comprehends isn’t all that important. Does he seem content? Maybe the sound of your voice is all that matters.
Contentment is what we are looking for here. Never forget how vulnerable this person is and that it is your responsibility to monitor the person’s body language. Chances are you’ll find that you have some memorable moments with your elder if you put your mind to it. Careful, light massage with a pleasing lotion or oil, holding a hand, reading, singing, playing music, praying aloud – all of these things will add quality to your visit. It definitely beats sitting there watching the clock and wondering if you are just wasting your time with the visit.

Why are Lasting Powers of Attorney important for carers?
In a recent YouGov survey, commissioned by Carers Trust, 82% of respondents had not made an LPA. Of those who had made provisions, few realised the importance of having both a ‘Property and Financial Affairs’ LPA, which gives someone the power to act on your behalf to make decisions about your property and financial affairs; and a ‘Health and Welfare’ LPA, which means that someone else has the power to make decisions about your personal welfare and healthcare when you are unable to do so.
Carers have spoken of their concerns that completing an LPA can be complicated, time consuming and expensive. While it is true that it takes a little time and there is a cost involved, carers have told us that the benefits outweigh the cost in time, money and stress later on. OPG has recently reduced the cost of registering an LPA and people on low incomes can apply for an exemption or reduction of the full fee.
Carer speaking about their experience; “This [LPA] should be a priority right at the start. Without a lasting power of attorney you cannot do anything. Everyone should be informed about both types of LPA, financial and health, from their 40th birthday. It was too late to get power of attorney by the time diagnosis was given to Dad, which caused problems and financial hardship. We were unable to access his savings account when he needed a ramp to get outside, and had to use a credit card for expenses which, obviously, cost more.â€
Having an LPA in place to appoint a carer as an attorney for the person they care for has vital practical, as well as emotional, implications. It allows the carer to carry out the wishes of the person they care for when it comes to their treatment and care, gives access to the person’s finances to pay for equipment, adaptations and formal support; as well as helping to safeguard against fraud. Having an LPA in place helps to include the carer and enables them to feel more confident in what may at first feel like an overwhelming situation, such as making decisions about residential care and end of life care.
A health and welfare LPA can’t be used until it’s proven that the person has lost mental capacity. A property and finance LPA can either be used when a person has lost mental capacity, or while a person still has capacity, with their permission, e.g. if they would like somebody to collect their benefits/pension or pay their bills on their behalf.
“My husband and I discussed everything when he first had a diagnosis, we recorded his wishes and put an LPA in place before he lost the capacity to make decisions. It gives me such peace of mind; I know what he would want and it means the family and professionals are also aware, therefore, there are no problems†(Carer)
If you would like to find out more, Carers Trust, in partnership with Sitra and Care Charts UK, have developed a free guide to the Mental Capacity Act for carers which gives more information about Lasting Powers of Attorney. There is also information on Carers Trust website here about the application process.

Carers at ‘breaking point’, with one in four reporting they’ve not had a single day off in five years
Carers are reaching “breaking point†as they struggle to take even one day off for years at a time, research by Carers UK has found. Seven thousand carers nationwide participated in a survey carried out by the charity.
‘Catastrophic impact’
Overall, 40 per cent of unpaid carers have not had a break in over a year, while 25 per cent have not had a single day away from caring in five years. This figure rises to one in three when the answers of long-term carers only are taken into account.
Nearly nine out of 10 (87 per cent) of carers struggle to get any form of respite from their responsibilities, according to the findings, published on Tuesday in the 2017 Carers UK “State of Caring†report.
The charity pointed to the “catastrophic impact†of giving constant care 365 days a year.
Carers who had not had a break in a year or more reported a deterioration in their health, both mentally (73 per cent) and physically (65 per cent).
‘Breaking point’
Heléna Herklots, chief executive of Carers UK, urged the Government to improve support for carers, warning: “Without access to breaks, carers can quickly reach breaking pointâ€.
She said: “Carers are struggling to get a break because appropriate support for their loved ones isn’t available or services they rely on are being cut or charged for.â€
Some 6.5 million people in the UK provide unpaid care by looking after an ill, older or disabled family member, friend or partner, and 1.4 million people provide over 50 hours of unpaid care per week. Surviving on a pittance But while the UK’s unpaid carers save the economy an estimated £56.9bn per year, according to the ONS, they are entitled to just £62.70 per week Carer’s Allowance for a minimum of 35 hours work – the equivalent of £1.79 per hour.
Almost half (48 per cent) of carers responding to the survey reported living on a household income of less than £1,500 per month. “The Government has no understanding that so many carers have to use up all their savings and investments just to make ends meet,†said one respondent. “Carers are saving them millions and millions of pounds in caring for their loved ones, yet struggle to even receive a mere pittance [of benefits].†A spokesman for the Department of Health said: “We are committed to improving social care, which is why we will consult later this year and put it on a stable footing for the future.â€

Your Rights as a Family Carer – New CQC Leaflet
Carers play an important role in working with care providers and can often provide expert knowledge about the needs and behaviour of their loved one. Carers also have certain rights that are set out in the NHS Constitution.
However, we know that in too many situations hospitals are not providing adequate family or carer support. The CQC’s review of care between hospitals and care homes for people with dementia found that 61% of inspected hospitals did not adequately involve patients or their families in care decisions.
This project is part of the CQC’s commitment to gather feedback from people about their experiences of care. Visit the CQC’s website to find out how you can have your say on the subject of carers’ rights.

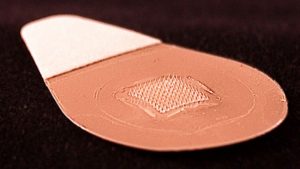
Painless flu jab patch for people scared of injections
The patch has a hundred tiny hair-like microneedles on its adhesive side that penetrate the skin’s surface.
It is simple enough for people to stick on themselves.
That should help more people get immunised, including those who are scared of injections, experts told the Lancet journal .
Bye bye injections
Unlike the standard flu jab, it doesn’t need to be kept in the fridge, meaning pharmacies could easily stock it on their shelves for people to buy.
It offers the same protection as a regular vaccine, but without pain, according to its developers from Emory University and the Georgia Institute of Technology, who are funded by the US National Institutes of Health.
The patch punctures the uppermost layers of the skin, whereas regular flu injections go all the way through and into muscle.
Lead researcher Prof Mark Prausnitz, who is also part of a company that wants to license the technology, said: “If you zoom in under the microscope what you’ll see are microscopically small needles. They puncture painlessly into the skin.”
His team tested the patch alongside flu injections. Some of the 100 volunteers got the regular shot in the arm, while others applied the microneedle patch to their wrist for 20 minutes.
Most said using the patch was painless, but some experienced mild side effects – redness, itching and tenderness in the area of skin area where it had been applied. These symptoms got better on their own over days.
Easy to use
Experts say the patch could revolutionise how flu and other vaccines are given, although more clinical tests over the next few years are needed to get the patch system approved for widespread use.
Dr Nadine Rouphael, from Emory University, said: “We could envisage vaccination at home, in the workplace or even via mail distribution.”
The patch can be thrown in the bin after it is used because the microneedles dissolve away.
And because it can be safely stored for up to a year without refrigeration, it could prove extremely useful in the developing world.
Experts from Public Health England said it might also be good to use in young children, who tend not to like needles, although the UK has already introduced a nasal spray flu vaccine for them.
John Edmunds, an expert in infectious diseases at the London School of Hygiene & Tropical Medicine, said: “This study is undoubtedly an important step towards a better way to deliver future vaccines.”
Other researchers have also been looking at pain-free skin delivery. A flu shot syringe that uses a microneedle has already been approved for use in the US.
Scientists in Australia have been designing a nanopatch with even smaller needles.