Latest News
Carers sought for mental health research advisory group
The group provide advice and feedback to researchers working in mental health, and review the research priorities of the NIHR Maudsley Biomedical Research Centre, a research institute that is a partnership of SLaM and the Institute of Psychiatry, Psychology & Neuroscience at King’s College London.
Taking part in the group improves the rigour, quality and relevance of scientific research, ensuring that it is of the greatest benefit to people with mental health illness and their carers. Meetings are held once every two months on Wednesday afternoons (4 to 5.30pm) at the Institute of Psychiatry, Psychology & Neuroscience in Denmark Hill, London, and travel expenses and attendance can be reimbursed for group members.
If you care for somebody with experience of mental illness, or know somebody who does, and are interested in playing an active role in improving the quality and relevance of research into mental health, please contact Joanne Evans ([email protected]) to find out more.

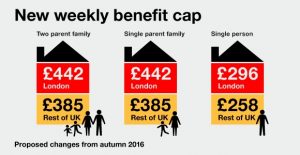
High court rules applying benefit cap to lone parents with children under two is unlawful
Upon considering the impact of the benefit cap, Mr Justice Collins concluded that “real misery is being caused to no good purpose.â€
The challenge was brought by four lone parent families. You can find out more about the decision on the Hopkin Murray Beskine website and the Garden Court Chambers website
A Department for Work and Pensions spokesman said:
“We are disappointed with the decision and intend to appeal. Work is the best way to raise living standards, and many parents with young children are employed.
The benefit cap incentivises work, even if it’s part-time, as anyone eligible for working tax credits or the equivalent under Universal Credit, is exempt. Even with the cap, lone parents can still receive benefits up to the equivalent salary of £25,000, or £29,000 in London and we have made Discretionary Housing Payments available to people who need extra help.â€
A previous High Court decision Hurley and others v Secretary of State for Work and Pensions found that the benefit cap was unlawful because it discriminated against those entitled to Carers Allowance who provide care to relatives such as a parent or grandparent, or a disabled child aged 18 or over. As a result of that decision the law was changed.
UK heart disease deaths fall by over 20% since indoor smoking ban
Deaths from heart disease and strokes caused by smoking have fallen dramatically since lighting up in pubs, restaurants and other enclosed public places in England was banned 10 years ago.
New figures have shown that the number of smokers aged 35 and over dying from heart attacks and other cardiac conditions has dropped by over 20% since 2007 while fatalities from a stroke are almost 14% down.
The statistics, which Public Health England (PHE) has shared with the Guardian, come as medical, public health and anti-tobacco groups prepare to mark the 10th anniversary next Friday of smoking being prohibited in indoor public places by Tony Blair’s Labour government on 1 July 2007.
Figures collected by PHE’s Local Tobacco Control Profiles network show that while there were 32,548 deaths from heart disease attributable to smoking in 2007-09, there were 25,777 between 2013 and 2015 – a fall of 20.8%. Similarly, a total of 9,743 smokers died from a stroke in 2007-09, but fewer – 8,334 – between 2013 and 2015, a drop of 14.5%.
Duncan Selbie, PHE’s chief executive, hailed the figures as proof of the ban’s huge beneficial impact on health. “The law has played a key part in the huge cultural change we have seen in the past decade, especially among younger people, a change that has literally saved thousands from disabling chronic diseases and premature death,†he told the Guardian.
“The smokefree legislation has been extraordinary in the way we now experience and enjoy pubs, clubs, restaurants and so many other public places. It was undoubtedly the single most important public health reform in generations,†he added.
The decline in smoking-related heart deaths is especially significant because smoking still accounts for about one in every six deaths in England – about 79,000 people a year. Fatalities due to heart disease make up a substantial proportion of them. Smoking-related deaths are three times more likely to occur among poorer people than those from better-off backgrounds, research showed.
The Health Act 2006, which introduced the ban in England, was the first of 10 pieces of legislation over 10 years that have helped drive down smoking’s popularity to its lowest level ever, Selbie said. The numbers of people across the UK who smoke has fallen over the last year from 17.2% to 15.8%, according to the most recent figures from NHS Digital, published last month.
England was the last UK nation to bring in a ban. Scotland did so in March 2006 and Wales and Northern Ireland followed in April 2007. The Blair government initially considered exempting bars, private clubs and pubs where no food was served. But it instead decided to impose a blanket ban after MPs and doctors criticised the exemptions as unfair, unworkable and likely to harm the health of staff breathing in secondhand smoke in premises where smoking continued.
“We’ve seen cigarettes stubbed out in public places, become far less visible in shops and had large graphic warnings put on packs starkly explaining what these things do to the human body – and all the misery and death they cause,†added Selbie.
“Its legacy has had a phenomenally positive impact on societal attitudes to smoking. Smokers have seized the opportunity by quitting in unprecedented numbers and of those still smoking, half have chosen to smoke outside their own homes to protect their families from secondhand smoke.â€
Although fewer people than ever still smoke, PHE is concerned that it remains much more common among certain groups, including younger women, and is a major source of health inequalities.
For example, while just 10% of married people smoke, 21.2% of those who are single do so, as do 18.8% of those who have been widowed, divorced or separated. And while 15.7% of people who live with others smoke, 27.8% of those living alone light up. And the jobless, those in routine and manual jobs and those without a degree are between two and three times more likely than the employed, those in managerial and professional roles and graduates to use cigarettes.
“The decline in deaths since 2007 from smoking-related heart attacks and strokes shows the effectiveness of a comprehensive approach by government to tackle smoking,†said Deborah Arnott, chief executive of the charity Action on Smoking and Health.
“But there are still over 30,000 premature deaths a year from smoking-related heart attacks and stroke, and the government strategy for tackling this public health epidemic expired at the end of 2015. We need an ambitious new government strategy to be put in place immediately if deaths from smoking are to decline as fast in the next decade as they have in the last.â€

Government must let service users and carers shape social care policy
There can be no question that Theresa May’s disastrous social care manifesto policy played a major part in her election failure. However, the Queen’s speech suggests that she still far from finding a sustainable way forward for social care that will command popular support. The speech only included 14 vague and non-committal words on the subject: “My ministers will work to improve social care and bring forward proposals for consultation.â€
Not only does this highlight the insecurity of her government and leadership. Much more importantly, it emphasises that any political party wanting to win the next general election will have to be prepared to listen carefully to service users and carers when developing their future social care policy proposals.
For all the talk of user involvement in health and social care, it hasn’t really happened in the past, but is clearly critical now. After the “dementia tax†debacle, no sensible politician is going to treat social care in such a cavalier fashion as May’s election team did. But taking it more seriously and giving it more priority is not enough on its own. Part of the problem has been that since Margaret Thatcher’s 1990 community care reforms, policymakers’ eyes have often been off the ball, because they have been at least as concerned with ideological commitments to privatising social care [pdf] as they have been with making it workable for people.
Thus the failure of prevention and personal budget policies and the continuing over-high levels of institutionalisation among older and disabled people. While there has been a lot of talk about the need to “integrate†health and social care policies, the same has conspicuously not been true of welfare reform and social care, with the former increasingly taking money away from disabled people and other long-term service users and making their lives more precarious, damaged and dependent.
The abrupt ending of a majority Conservative government committed to austerity and neoliberal small state politics creates a new opportunity to listen to service users and user-led organisations, as well as emphasising the critical importance of doing so. They have long been the most creative and innovative social care thinkers.
First they have repeatedly stressed the importance of putting social care on the same financial footing as the NHS if it is to meet the needs of the UK’s demography, which includes much greater numbers and proportions of older and disabled people. A diverse range of service users were brought together by Shaping Our Lives, supported by the Joseph Rowntree Foundation in 2009, to explore proposals for funding social care for the future. They felt that a false divide between social care and health care was perpetuated by conflicting funding arrangements. Almost all thought general taxation was the best way to fund social care.
But this is only the beginning of the story. Social care service users – including people with learning disabilities, sensory and physical impairments and long-term conditions, as well as mental health service users – all stress that a much more social approach to care (and welfare benefits too) is needed. It should get beyond individual medical conditions and see beyond pathologising the individual for what they can’t do and support them to do all they may be able to. Our health and social care systems don’t currently do this. They don’t come in to help to maximise people’s opportunities to contribute – through work, family, involvement in their community – only when they judge they “can’t manage†any more.
For years the disabled people’s movement has tried to change our understanding of “independent living†from a traditional idea of “standing on your own two feetâ€, to having support to live life on as equal terms as possible with other people. But still our health and social care system are stuck in the past. The political party that wins the next general election is likely to be the one that signs up to this new vision of social care and support. And that will be the party that really does its homework, stops prevaricating, listens to service users and carers and their organisations and involves them fully and equally in its policy process.

Eligible for carer’s credit? Don’t put your state pension at risk by not claiming it
Carer’s credit is not a typical benefit, as you don’t receive any money for it. However, it’s important to claim it – otherwise your state pension could be negatively impacted.
- Carer’s credit is a national insurance ‘credit’ designed to fill gaps in your national insurance record (eg, from having to give up your job to care for someone).
- It’s this record that determines if you’ve worked enough to earn the state pension.
- You could get it if you care for someone for at least 20 hours a week.
According to new figures from the Department for Work and Pensions, it’s estimated up to 250,000 carers are eligible to claim carer’s credit – but just 20,000 are actually doing so.
Charity Carers UK puts the total number of unpaid carers in the UK at 6.5 million – if you’re one of those and think you could be eligible for carer’s credit, it’s important to check now if you can claim.
Heléna Herklots, Carers UK chief executive, told us: “When people take on a caring role for a loved one, they can face serious financial hardship. Many carers see a steep drop in income if they have to leave work or reduce their hours to care.
“It is vital that carers are able to protect their state pension entitlement and don’t suffer an ongoing impact from reducing hours or leaving work to care.”
How is carer’s credit different from carer’s allowance?
Carer’s allowance, worth up to £62.70 a week, is a totally separate benefit to carer’s credit.
- To qualify for carer’s allowance, you must care for someone for at least 35 hours a week although you don’t have to be related or live with them (see full eligibility criteria).
- If you’re eligible for and receive carer’s allowance you’ll automatically get carer’s allowance credit, which works in the same way as carer’s credit – so there’s no need to worry about claiming for carer’s credit too.
How to apply for carer’s credit (Not sure if you’re eligible? Still apply)
We explain how to check if you’re eligible for carer’s credit below. But in short, if you don’t get carer’s allowance and you do care for someone then apply anyway.
There’s no harm in doing so if you’re unsure whether you’re eligible – the worst that’ll happen is your application will be rejected.
The application process is straightforward: you can download a carer’s credit application form or call 0345 608 4321 to get one. You then need to fill it in and post it to the Government’s carer’s allowance unit.
Your application must be received before the end of the tax year following the tax year to which the credits relate. This means a claim for the 2016/17 tax year (the last tax year) must be made by 5 April 2018.
How will I know if I’m eligible for carer’s credit?
To get carer’s credit you must fulfil the following criteria (though if you’re unsure on anything, contact the carer’s allowance unit on 0345 608 4321):
- You must be aged between 16 and state pension age.
- You must look after one or more people for at least 20 hours a week. You don’t get more ‘credits’ if you look after more than one person.
- The person you’re caring for must also receive at least one of these benefits: disability living allowance (care component at the middle or highest rate), attendance allowance, constant attendance allowance, personal independence payment (the daily living component at the standard or enhanced rate) or the armed forces independence payment.
- If the person you’re caring for doesn’t receive one of these benefits, you could still be eligible for carer’s credit – but you’ll have to get a health or social care professional to sign the application form to verify it.
- You can also still get carer’s credit if you have breaks from caring (up to 12 weeks in a row), such as if you take a holiday, go into hospital or the person you’re caring for goes into hospital.
- Bizarrely, it’s possible for two people fulfilling the criteria above to be eligible for carer’s credit by caring for each other.
Can I claim carer’s credit for previous years?
Yes – you can go back one year, which means a claim made by 5 April 2018 could go back as far as the beginning of the 2016/17 tax year. You can also claim retrospectively even if the person you were caring for has since died or no longer needs caring for.
In these situations it’s best to contact the carer’s allowance unit on 0345 608 4321.
What other help is there for carers?
This week is Carers’ Week – an annual campaign to raise awareness of caring and the challenges faced by carers.
The Care Act 2014, which came into force in April 2015, sets out carers’ legal rights. Part of it includes giving carers a right to request a ‘carer’s assessment’ from their local authority.
This assessment is carried out by a professional from your council who will work out how being a carer affects your life and assess what the council can do to help that.
Young carers (aged under 18) can also apply for an assessment. For more information, see guidance from the Carers Trust and the NHS.
For help and support, carers in England can also call the NHS Carers Direct helpline on 0300 123 1053. For other parts of the UK (although it covers England too), Carers UK has a free advice line on 0808 808 7777.

Catheter Care Awareness Week
Catheter Care Awareness Week is about empowering patients and professionals to question current practices, improve their knowledge, and reduce the stigma associated with catheters.
We have developed a digital pack, available on their website for you to share with staff, patients and carers, containing information about the project, our shared aims, and how to get involved. The pack contains:
- Their animation
- Patient stories
- Information on social media and suggested tweets using our hashtag #cathetercare
- Pledge cards and some suggested pledges
- Poster templates: a general one and one where you can add your own event information, for you to download and print.
- An internal communications piece for you to amend and share
- Films and vlogs about our project and the current challenges and improvements around catheter care which can be found here

SuperCarers: the startup that’s championing a new way to care for the elderly
Adam Pike and his brother Daniel were still quite young when their grandmother was diagnosed with dementia. She wanted to stay at home, but this was some distance from where the Pikes lived and they didn’t have enough money to hire private carers.
At first the family relied on local authority carers, then the brothers’ mother took over. But when their grandmother flooded her home for a second time, the family decided to look at residential care. “My grandma made my mother feel guilty for that choice until the day she died,†Adam Pike remembers. “It is a feeling that my mum lives with ten years on.â€
Today there are two million people elderly people in the UK who have a care related need. More than half of those, like Adam Pike’s grandmother, are unable to afford adequate personal care, but surveys show 90 per cent of over-50s would prefer to stay at home even they need care. Realising they weren’t the only family to suffer, Daniel and Adam Pike created SuperCarers. The platform provides an alternative to private home care and local authority services by linking carers and families online and letting the two parties arrange the terms of care.
“What we’re doing is reducing the high overhead costs of agency businesses by using technology,†Adam Pike says. “By connecting the families and the carers directly, the carers get paid the living wage and the families are saving money.â€
Agencies have higher overheads because they manage carers on behalf of families, acting as an employer. SuperCarers is classed as an introductory service because it does not direct or manage care. As such, it is not registered with independent regulator the Care Quality Commission.
Pike says this cuts out the middleman, giving families a more direct relationship with carers and removing the frustrations that some families feel when smaller agencies can’t immediately respond to issues. “The families get frustrated about the care coordinator who sits in the middle,†Pike says. Their research shows most people want to have the choice and control associated with private care, without compromising on quality.
Families also pay less and carers earn more, Pike says, because SuperCarers does not take a cut. Carers are free to set their own rate, factoring in tax and other payments that they have to make as a self-employed person. The average rate is £16 for a single hour of care. “We are clear with them,†Pike says. “We ask them to tick [a box to acknowledge] that they understand their employment status.â€
Not everyone is sold on the model. “I am yet to be convinced that there is such a thing as a self-employed care worker,†says Colin Angel, policy and campaigns director for the UK Homecare Association. “It probably is possible, but in my view the care worker is likely to be employed either by the person using the service or the organisation introducing them.â€
Angel says one major problem is that regulation hasn’t kept up with new models such as the introduction-only model used by SuperCarers: “They are offering one alternative among many but they are not offering the managed care service that most people in this country are using and expect. It’s certainly not the model that most local authorities are purchasing.â€
UKHCA has called for the Government to review its regulatory regime to take into account new models of care as the number of over-75s in the UK grows from 5.4 million in 2017 to 7.5 million in 2027. It has also called for the Government to create more stable funding for state-funded care. In its 2017 manifesto, the UKHCA says the Government should require local authorities and clinical commissioning groups to work with providers to understand, publish and pay the real costs of care.
SuperCarers was founded on the principle that current forms of funding are inadequate. “Care associations pay their members so poorly because the local authorities’ budgets are so small,†Pike says. “UKHCA say that for a care worker to be paid a living wage, the local authority must pay the agency £21 an hour, which is 50 per cent more than they are able to on framework agreements.â€
Pay is so poor, agencies are exiting the business. Plus by 2020 there will be 62,000 fewer carers in the UK because of changes to immigration, while demand is accelerating. Pike says SuperCarers is one of the few businesses attracting people to the profession.
SuperCarers now has about 650 carers on the platform offering day and night care in London and live-in care nationwide. It has an impressive roster of advisors, including Alan Rosenbach, who was director of strategy at the Care Quality Commission; Paul Burstow, former Minister of State for Community and Social Care; Jan Burns MBE, chair of the National Dignity Council; and Andrea Pope-Smith, a former director of Adult Social Services at two councils.
Last October, SuperCarers raised £1m on Seedrs, an equity crowdfunding platform. Investors include JamJar Ventures, a fund run by Innocent drinks company founder Richard Reed, and Chris Kelly, a paediatric junior doctor at St Thomas’ Hospital in London, who invested money from an online advertising company that he created in his first year of medical school and sold in 2008.
Kelly knows first hand the difficulties of discharging elderly patients because of the poor availability of at-home care. “You’re trying to discharge patients and the package of care isn’t enough. They wait for weeks on a ward while the local authority thinks about organising care and you think, there must be a better way to do this,†he says.
For SuperCarers to become the solution, it must first become recognised by regulators and the NHS. “The NHS favours large companies that they already have relationships with, rather than small ones,†Kelly says. “It’s very hard to penetrate. There are lots of policies being discussed that could change this, but it moves quite slowly. That’s one of the challenges.â€
Until then, elderly people continue to spend 445,000 days a year in hospital because of the lack of at-home care, according to the UKHCA. Kelly says: “SuperCarers is one way to help this problem that’s only going to get worse.”

Carers Week 2017
The vast majority of the UK public feel those caring unpaid aren’t sufficiently valued by society.
More than 7 in 10 (74%) of the UK public feel carers are not suf ciently valued by society for the support they provide and this gure rises to 8 in 10 (83%) of those who have previous experience of caring themselves but don’t currently.
The public are not prepared for a future caring role.
Half of respondents with no experience of caring (50%) think it’s unlikely they would ever become a carer.
When asked to choose their top three, worries about becoming a carer were affordability of care and the impact on their nances (46%) and coping with the stress of caring (43%).

Call for action: Stocktaking study on the needs of family carers
Families in Europe are greatly affected by current social and demographical changes, such as the growing ageing population, changing family structures, or the situation of intergenerational families. The purpose of this data collection is on one hand, to explore some of the challenges faced by family carers in accessing adequate resources, services, or time arrangements in different EU Member States. On the other hand, we hope to find some good examples of national, or local policies that help family carers to balance their work, family and personal life.
Target group: Family carers, informal carers and people from different EU Member States who are fulfilling a caring role towards a member of their family.
Languages: The questionnaire is available in English, German, Dutch, French, Italian, Portuguese, Spanish, Slovenian. However, we would be happy to receive answers from any other EU countries.
Data collection: From 15 May to 30 June 2017.
Questionnaire links:
If you are a family carer, please take a few minutes and fill out our online questionnaire. Every opinion counts!
Help COFACE Families Europe and COFACE Disability to shape our EU advocacy by bringing the most pressing challenges faced by family carers to the attention of decision-makers!
For any questions, please do get in touch with Magdi Birtha at [email protected]
More information about the International Day of Families 2017: “Families, education and well-beingâ€
Social Media : #DayOfFamilies @UNDESA @COFACE_EU

Kings College Hospital 2017 Elections to the Council of Governors
